“There’s a little bit of embarrassment with it,” Kendra Klamm, a sophomore in the College of Business Administration, says.
Klamm hasn’t always been in this position. For most of her life, when the need arose for her to visit a doctor, she could do so without any worry. When her father lost his job in January, and his health insurance plan along with it, Klamm’s situation changed. Klamm doesn’t talk about this part of her life often. She says no one would know unless they asked.
Klamm says that her family had a sense that her father was about to lose his job, so it gave them some time to figure out a plan in case somebody in the family became sick, but the uncertainty was still a point of anxiety.
“It forced me to take care of myself more,” she says.
A large portion of Americans, roughly 49 percent, receive health insurance from their employers. Had her father not lost his job, Klamm would have been able to stay covered under his insurance until she was 26 years old under the Affordable Care Act. But now she says she’s looking forward to graduating and finding a job that will offer her health insurance of her own.
Klamm’s family was able to find some security through a Christian healthcare sharing network called Samaritan Ministries. The idea is that Samaritan members are part of a community of uninsured who, by virtue of membership and paying a monthly share, are able to receive help from other members with the cost of care. So if Klamm were to need medical attention, other members in the network would be able to take some of the burden of her costs, under the presumption that the shares Klamm’s family pays each month would serve the same purpose for other members in the network.
There are limitations to the care Samaritan Ministries members are able to ask for help with, including minimum and maximum costs and restrictions on pre-existing conditions, like diabetes. Still, Klamm says the program gave her family members a sense of security when they were most vulnerable.
Klamm is one of a shrinking but significant group of college-aged adults without health insurance. In 2016, 13 percent of Americans between 19 and 25 years old were uninsured, the second-largest age group of uninsured, according to a 2017 U.S. Census Bureau report. The largest group of uninsured was adults 26 to 34 years old, at roughly 16 percent.
When the Affordable Care Act was signed into law in 2011, the percentage of uninsured Americans dropped from 18 to about 11 percent. In 2017, that number was up to just over 12 percent.
The ACA contributed to this drop in a number of ways, Marquette University political science professor Philip Rocco says. Perhaps the most significant impact of the Affordable Care Act was the option it gave states to expand Medicaid programs for their residents, Rocco says.
Medicaid, a state and federally funded health insurance program for low-income Americans, covers more than 72 million people nationally. Whether a person qualifies for Medicaid depends on a number of things, Rocco says, including the state that person lives in and their income level. While Medicaid is an option for many low-income Americans — around 19 percent of the U.S. population — it doesn’t cover everyone.
Dr. Thomas Bachhuber of Sixteenth Street Community Health Centers says that the answer to some of these questions might not start at big health systems, but at local, community-based organizations like his. Sixteenth Street provides low-cost primary health care for a person’s entire lifetime. While it originally started in 1969 with a few nurse practitioners, a midwife and a family practice doctor, it has since expanded to provide mental health services.
“You won’t find this kind of support in a private office,” Bachhuber says. “The structure allows us to keep everybody within house.”
Sixteenth Street provides rates to patients on a sliding scale, meaning that their income is measured using the federal poverty line as an index for affordable care. This has resulted in copays as little as $5 for patients who are completely below the poverty line. According to the Sixteenth Street 2016-’17 annual report, 65 percent of its patients were 100 percent below the poverty line. Due to partnerships with hospitals like Columbia St. Mary’s, Sixteenth Street can refer patients to hospitals that will also honor the sliding scale. Bachhuber says, however, that the sliding scale system is not without its drawbacks.
“The sliding cost system really doesn’t help the people in the middle,” Bachhuber says. “People who are above the poverty line but also not able to afford the full coverage are really feeling it. People are falling through the cracks.”
Bachhuber says the Affordable Care Act provided more options for people in the middle, before rollbacks gutted the program. He also says that a universal healthcare option should be explored to help people caught in the middle.
At Sixteenth Street, waiting is a common theme. High demand for low-cost care often fills the waiting room and queues with patients. Bachhuber says Sixteenth Street often prioritizes the need for urgent care, but it tries to retain as many patients as possible.
“We’re always playing catch up,” Bachhuber says. “People don’t leave as much as they come in.”
While Sixteenth Street does not make much money, it has made a significant impact in the community. In 2016-’17, 37,821 patients used its myriad services, according to the clinic’s annual report. Over the past year, it hired mid-level prescribers and specialists to improve its network of care.
“We’re not out to get a ton of money,” Bachhuber says. “We’re here to do great work.”
While Bachhuber says he believes community-based health models would help with insurance rates, he also says there would need to be a surge in manpower to staff them.
“A lot of students are going specialty,” Bachhuber says. “We’re just not the sexy pick right now.”
But for those navigating the demanding experience of being a college student alongside the burden of finding affordable medical treatment when they need it, a variety of programs exist.
The problem, says Steve Ohly, a nurse practitioner with Aurora Health Care and founder of the Walker’s Point Community Clinic, is that people don’t know these programs exist, or worse, they don’t seek treatment at all because of anxiety about cost.
Ohly says helping patients understand their options is a large part of what they do at the clinic.
“It’s because of that anxiety that they come to us,” he says.
Ninety-five percent of Ohly’s patients are uninsured, and the clinic provides treatment for little or no cost, but he says he rarely sees students. The reason, he says, is because students will usually go to their campus health clinics.
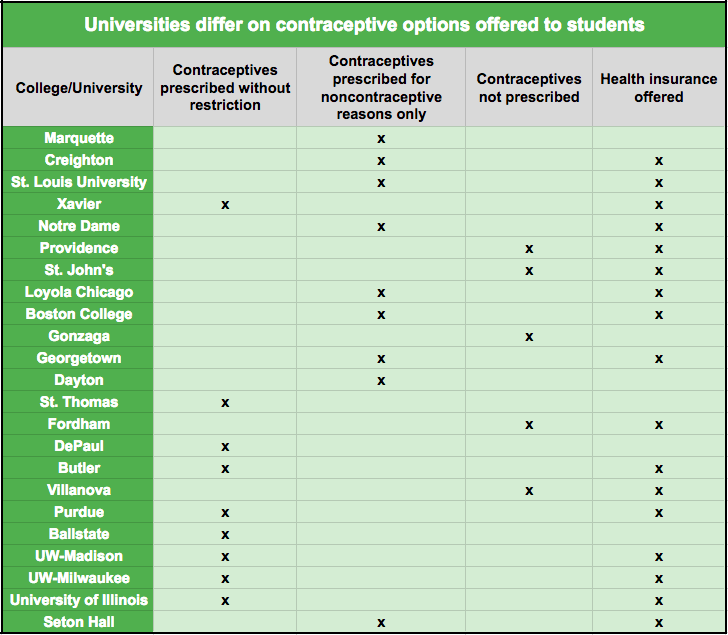
At Marquette, that clinic is run by Dr. Robin Brown. The Marquette University Medical Clinic provides a number of services, including running blood tests, STI screenings, immunizations — like flu shots — and X-rays. Students can make appointments online, and same-day visits are allowed for urgent care situations.
Rocco says if students need more care than a clinic can provide, they may qualify for Badgercare, Wisconsin’s version of Medicaid. The program was started in 1999 and Wisconsin residents, which may include Marquette students with permanent addresses, can apply to benefit from the coverage.